Table of Contents
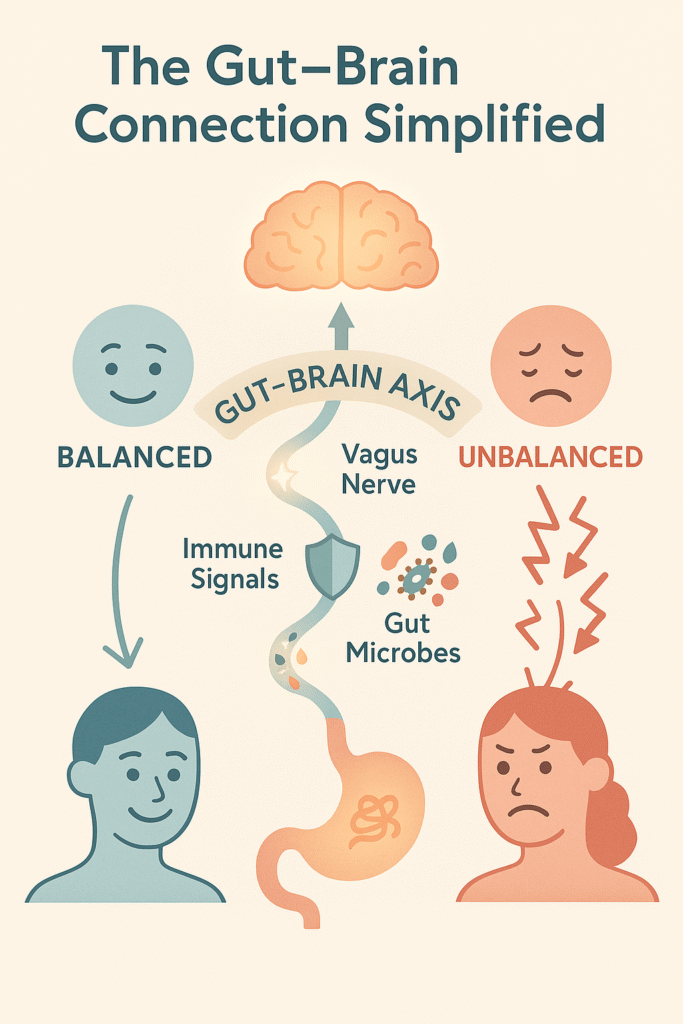
Ever had a stressful day that left your stomach in knots—or found that ongoing tummy troubles dragged your mood down? That’s no coincidence. Your gut and brain are in constant conversation through what’s called the gut–brain axis. This two-way link runs on nerves, hormones, and even the trillions of microbes in your digestive system.
When the system is balanced, digestion feels smooth—less bloating, fewer cramps, more regularity—and your mood is calmer too. But when stress hits, the signals get scrambled. The result? Gas, bloating, cramping, or even bathroom changes that often come with anxiety or irritability.
The good news: nature offers gentle allies. Certain herbs for digestion can soothe the gut directly while calming the stress signals that make symptoms worse. From peppermint and ginger to chamomile and ashwagandha, research shows that the right plants can ease bloating, reduce cramps, support regularity, and help your mind and gut feel more at ease.
In this guide, you’ll discover the best herbs for gut health, how they work with the gut–brain connection, and safe, practical ways to try them for real relief.
What Is the Gut–Brain Axis? (Explained Simply)
Your gut and brain are in constant conversation — and they don’t need words to talk. Instead, they use a few key “channels” to send messages back and forth:
The vagus nerve 🧠: Think of it as a direct phone line between your gut and your brain. Signals can travel both ways, letting your brain know when your stomach is full or when it’s in distress.
Your immune system 🛡️: When there’s stress, irritation, or inflammation in the gut, your immune cells send out chemical “alerts” that the brain quickly picks up on.
Gut microbes and chemicals 🦠: Trillions of bacteria live in your intestines, and they produce substances like short-chain fatty acids and serotonin-like chemicals that can influence mood and gut function.
When these pathways are in balance, digestion tends to run smoothly: less bloating, steadier bowel movements, and a calmer mind. But when the system is out of sync, the same signals can cause problems. You might notice stomach pain, nausea, or sudden bathroom changes — often paired with anxiety, low mood, or that familiar “gut feeling” of stress.
This two-way link is why researchers call the gut–brain axis a “conversation.” And just like in any relationship, when the lines of communication are clear, everything feels better. When they’re scrambled, both digestion and mood can suffer.
Herbs for IBS, Bloating, and Cramps
Peppermint Oil for IBS Relief
If you’ve ever felt your stomach twist and cramp for no clear reason, you’re not alone. For many people with IBS, the gut muscles tighten more than they should — leading to pain, bloating, and irregular bowels. That’s where peppermint oil comes in.
Peppermint naturally relaxes smooth muscles in the digestive tract, helping ease those spasms that trigger cramps. Think of it as gently telling the gut to “take a breath.” This is why peppermint has been used for centuries in digestive remedies.
And modern research backs it up. Clinical studies — including recommendations from the American College of Gastroenterology — suggest that peppermint oil capsules can improve global IBS symptoms, reducing both pain and bloating. In fact, several reviews have found peppermint outperforms placebo when it comes to easing IBS discomfort.
But not all peppermint is created equal. Regular capsules can release oil too early, irritating the stomach or worsening reflux. Enteric-coated peppermint oil capsules are the better choice. These pass through the stomach intact and release their soothing effects in the intestines, right where they’re needed most.
Practical tip: If you struggle with IBS cramps or bloating, try a reputable enteric-coated peppermint oil supplement. Start with the lowest dose recommended on the label and give it a couple of weeks to see how your body responds. Many people notice fewer cramps and less bloating when taken consistently.
Peppermint + Caraway (Menthacarin) for Functional Dyspepsia
If you’ve ever felt uncomfortably full after just a few bites, or dealt with nagging pressure in your upper stomach without obvious heartburn, you might be experiencing something doctors call functional dyspepsia (FD). It’s a fancy term for a very real kind of upper-digestive discomfort — that heavy, tight, or burning feeling that can sneak in even when tests don’t show anything “wrong.”
Here’s where a blend of peppermint and caraway oil, often sold under the name Menthacarin, comes in. This herbal duo has been studied in people with FD, and the results are encouraging. In clinical trials, those who took the combination noticed lighter feelings of fullness, less stomach pressure, and overall relief compared to people who took a placebo. Researchers believe peppermint helps relax the digestive tract while caraway reduces gas and bloating, making them a powerful team for stubborn upper-belly discomfort.
How you might use it
If you’ve tried peppermint on its own and didn’t get full relief, or if your main issue is that heavy, “food just sits there” feeling, peppermint + caraway may be worth considering. Most studies use standardized capsules rather than teas, since the precise blend and dose matter. Look for products labeled enteric-coated — this helps the oils reach your intestines where they can do their best work, while reducing the chance of peppermint causing heartburn.
As always, it’s smart to check in with a healthcare professional before starting any supplement, especially if you’re on medications or managing other health conditions. But for many people, this simple herbal pairing has brought welcome relief and made meals feel lighter and easier to enjoy.
Digestive Bitters: Natural Support Before Meals

Ever notice how just the smell of food can make your mouth water and your stomach start to “wake up”? That’s your body kicking into what’s called the cephalic phase of digestion — basically, your system’s way of warming up before a meal.
This is where digestive bitters come in. Herbs with a naturally bitter taste — like gentian, wormwood, artichoke, and dandelion — can gently trigger those same digestive reflexes. By simply tasting a small amount before eating, you nudge your stomach to produce more digestive juices, improve blood flow to the gut, and help your body break down food more smoothly. For many people, this translates into less bloating and less of that sluggish, heavy feeling after the first few bites.
How to Try Bitters
The easiest way to use bitters is as a liquid extract. A few drops or a small sip about 10–15 minutes before a meal is usually enough. You don’t need a large amount — it’s the taste that sets things in motion. If you’re new to them, start small and see how your body responds.
Multi-Herb Formulas: Iberogast (STW-5)
For people who deal with ongoing upper stomach discomfort, there’s also a well-studied herbal blend called Iberogast (also known as STW-5). It combines several bitter and aromatic herbs into one formula and has shown benefits in reducing symptoms of functional dyspepsia — that nagging sense of fullness, pressure, or mild pain after eating. Clinical studies suggest it can ease cramping and heaviness, making meals feel more comfortable.
Bottom Line
Digestive bitters are a simple, natural tool to “prime” your digestion before meals. Whether you try a single herb like gentian or a multi-herb option like Iberogast, they offer a gentle way to support your gut health without major changes to your routine.
Artichoke Leaf Extract for Bloating and Nausea 🌿
If you’ve ever felt heavy, bloated, or vaguely nauseous after meals — no matter what’s on your plate — artichoke leaf might be worth exploring. Unlike the vegetable you dip in butter, the artichoke leaf extract used in supplements has been studied for its digestive benefits, especially in people with upper-GI discomfort.
What the Research Says
In a well-designed clinical trial, people who took artichoke leaf extract for six weeks reported noticeable improvements in symptoms like bloating, nausea, and that lingering “full belly” feeling compared to those on a placebo. Researchers believe artichoke leaf may help by supporting bile flow — which your body uses to break down fats — and gently calming the digestive system.
How You Can Try It
If you often deal with post-meal bloating or upper-stomach discomfort, artichoke supplements may offer relief. Most studies have used standardized extracts, which means the active compounds are measured for consistency. Look for products that mention this on the label, and follow the dosing instructions provided.
A simple tip: try taking artichoke extract before your largest meal of the day. Some people notice that’s when it makes the biggest difference in easing fullness and queasiness.
Safety Notes
Artichoke is generally well tolerated. However, if you’re allergic to related plants (like daisies or marigolds) or have gallstone issues, check with a healthcare provider before starting. For most people, it’s a gentle, natural way to support smoother digestion.
Bottom line: Artichoke leaf extract may help ease bloating, nausea, and upper GI discomfort, making it a practical option for anyone looking to add natural support to their gut health routine.
Anti-Inflammatory Herbs for Gut Lining Health
Turmeric / Curcumin for Digestive Inflammation
If you’ve ever cooked with turmeric, you know it gives curry that golden color — but inside your body, it does more than brighten up a dish. The key compound in turmeric, curcumin, has strong anti-inflammatory effects. That matters because inflammation is at the root of many digestive issues.
Researchers have studied curcumin as a supportive add-on for people with ulcerative colitis and other inflammatory bowel conditions. In several clinical trials, people who took curcumin along with their standard medications were more likely to see their symptoms calm down — and in some cases, even reach remission — compared to medication alone. This doesn’t mean turmeric is a cure, but it does suggest it can be a helpful partner for gut health when used alongside medical care.
Practical tip: if you’re using turmeric in the kitchen, pair it with black pepper and a little healthy fat (like olive oil) — this helps your body absorb curcumin better. For stronger support, standardized curcumin supplements are available, though doses in studies are usually higher than what you’d get from food alone.
Safety note (in plain English): Curcumin can act a bit like a natural blood thinner. If you’re already taking medications such as aspirin, warfarin, or other anticoagulants, or if you have surgery coming up, check with your healthcare provider before adding high-dose supplements. For most healthy people, everyday culinary use is considered safe.
Bottom line: Turmeric and curcumin won’t replace your treatment, but they may help cool down gut inflammation and support a calmer digestive lining when used wisely.
Herbs for Gas, Bloating, and Post-Meal Pressure
Fennel for Bloating and IBS
If you’ve ever chewed on fennel seeds after a meal, you’ve already tapped into one of the oldest natural remedies for digestion. In many cultures, fennel has been used as a carminative herb — meaning it helps relax the digestive tract and ease gas. That simple tradition has stood the test of time because so many people find it soothing.
Modern research is starting to back up what folk wisdom has always suggested. In one study, people with irritable bowel syndrome (IBS) who took a blend of fennel essential oil and curcumin (the active compound in turmeric) reported less bloating, reduced cramping, and even an improved quality of life compared to those on a placebo. While the results came from a combination supplement, fennel’s role as a digestive ally is hard to ignore.
So, how might fennel help? Scientists think it gently stimulates the muscles in the gut, which keeps food and gas moving along more smoothly. That action can explain why fennel tea or capsules are often used to ease post-meal pressure, gas, and digestive sluggishness.
Practical ways to try fennel:
Sip on fennel tea after meals to reduce bloating.
Try fennel capsules if gas and cramping are ongoing issues, especially if you also deal with IBS.
Keep it gentle: start small, see how your body responds, and layer it into your routine as needed.
Fennel won’t “cure” digestive issues, but for many, it’s a safe, natural way to bring a little lightness back after meals.
Herbs for Nausea and Slow Digestion
Ginger for Nausea Relief
If your stomach often feels unsettled—whether from motion sickness, pregnancy, or even after certain treatments—ginger is one of the most trusted natural go-tos. For centuries, people have turned to this warming root to calm queasiness, and modern research backs it up.
Studies show that ginger can ease nausea linked to morning sickness, chemotherapy, and post-surgery recovery. It doesn’t work like a heavy-duty drug—it’s gentler—but for many people, that’s exactly the appeal. Instead of knocking out your system, ginger helps nudge your digestion back into balance.
Beyond nausea, ginger has also shown promise for functional dyspepsia (that lingering upper-stomach heaviness and discomfort that doesn’t always have a clear cause). In one study, people who took a ginger and artichoke extract combo reported less bloating and stomach pressure after meals.
So how can you use it?
Everyday support: A cup of fresh ginger tea—made by steeping sliced root in hot water—can be a soothing ritual.
More targeted relief: Standardized extracts (found in capsules or tablets) provide a consistent dose and are what most clinical studies use. These are a good option if you’re dealing with ongoing nausea or slow digestion.
Most people tolerate ginger well, and it’s easy to add into your routine—whether through tea, cooking, or supplements. If nausea or sluggish digestion regularly gets in the way of your day, ginger is a simple, safe herb to try.
Stress-Relieving Herbs for Gut–Brain Support
When stress kicks in, digestion often takes the hit. Your body shifts into “fight-or-flight” mode, which slows gut activity and tightens muscles in the digestive tract. That’s where calming herbs like chamomile and lemon balm come in. Both have been used for centuries as gentle, stress-soothing teas that also support the digestive system.
Chamomile for Calm and Comfort
Most people know chamomile as a bedtime tea, but it’s also a trusted herb for digestion. Research suggests chamomile can ease mild cramping and reduce excess gas, while also calming the nervous system. That makes it a great option if your stomach tends to knot up when you’re anxious. A simple cup of chamomile tea in the evening can do double duty—relaxing your mind while giving your belly some relief.
Lemon Balm for Stress-Sensitive Digestion
Lemon balm (Melissa officinalis) has a light, citrusy flavor and a long history as a “mood herb.” Modern studies show it may help lower short-term anxiety and improve sleep quality. For people whose digestion flares when stress runs high, lemon balm tea or tincture can gently take the edge off.
Practical Ways to Use Them
Chamomile tea 🍵: Brew a bag or a spoonful of dried flowers before bed to wind down and reduce nighttime bloating.
Lemon balm tea or tincture 🍋🌿: Try it in the afternoon or evening if stress triggers your stomach. It pairs well with chamomile in calming blends.
Both herbs are considered safe for most people, and they’re easy to find at grocery or health stores. If you’re looking for natural remedies for stress-related digestion, chamomile and lemon balm are simple, gentle places to start.
Ashwagandha for Stress-Sensitive Digestion
If stress tends to hit you in the stomach, you’re not alone. Many people with IBS or other digestive issues notice flare-ups right when life gets overwhelming. That’s where ashwagandha can play a role.
Ashwagandha is what’s called an adaptogen—a plant that helps your body handle stress more smoothly. Instead of pushing you one way or the other, it works like a stabilizer, gently balancing your stress hormones (like cortisol) so they don’t swing out of control.
What does that mean for digestion? When stress hormones stay in check, your body is more likely to stay in “rest-and-digest” mode instead of flipping into “fight-or-flight.” For people with stress-sensitive IBS, that can translate to fewer flare-ups, less urgency, and a calmer gut rhythm overall.
Research backs this up too. Clinical reviews and NIH reports suggest ashwagandha can lower anxiety and improve resilience to stress. While it’s not a cure-all, it’s a promising option if your digestion seems tightly linked to your stress levels.
Practical tip: Ashwagandha is usually taken as a capsule or powdered root mixed into warm drinks. If you’re trying it, start with the lowest dose on the product label and give it at least a couple of weeks to notice a difference. And because it can interact with certain medications or conditions, it’s smart to check with your healthcare provider first.
Bottom line: If stress feels like your digestive “trigger,” ashwagandha may help smooth out both your mood and your gut.
Licorice for Digestion: Choosing the Safer Form
Licorice root has a long history as a stomach soother. But in its natural form, it contains a substance called glycyrrhizin, which can cause problems like raising blood pressure and lowering potassium levels. Those changes may stress the heart and kidneys or clash with certain medicines.
Luckily, there’s a gentler version made just for digestion. It’s called deglycyrrhizinated licorice — or “DGL” for short. In this type, the risky compound is removed, so you still get many of the gut-calming benefits without as much concern about blood pressure or potassium shifts.
Some studies — both older trials and newer extracts like GutGard — suggest that this safer form of licorice may ease stomach irritation (gastritis) or ulcer-type discomfort. While the research isn’t as modern or large as we’d like, many people report it helps with burning, cramping, or unsettled stomach feelings.
How to use licorice for digestion safely:
Look for products labeled “DGL.” This is the safer form designed for stomach support.
Avoid if you have high blood pressure, kidney problems, or take medications that affect potassium or blood pressure.
Pair it with basics like steady meals, plenty of water, and stress care for best results.
In short: if licorice is on your radar for digestive relief, choose the safer “DGL” form and check with your healthcare provider first.
Safe Ways to Use Digestive Herbs with Practical Guide
When it comes to herbs, there’s no one-size-fits-all. The best results come when you match the right herb to the right symptom and use it wisely. Here’s a simple framework to help you get started:
1. Match the Herb to Your Symptom
Think of herbs as tools in a toolbox. Each one shines in a different situation:
Peppermint oil is a top choice for IBS-related bloating and cramping.
Fennel and curcumin work well together if gas and fullness are your main complaints.
Ginger is your go-to for nausea or queasiness.
Chamomile, lemon balm, and ashwagandha are especially helpful if stress seems to trigger your digestive flare-ups.
By picking the herb that fits your pattern, you’re much more likely to notice real relief.
2. Start Low, Go Slow
Your gut needs time to adjust. Begin with the lowest dose suggested on the product label. Stick with it for two to three weeks before deciding whether it’s helping. This gentle, patient approach makes it easier to spot what’s truly working (and avoids overloading your system).
3. Choose Quality Products
Not all supplements are created equal. Look for:
Enteric-coated peppermint oil (so it bypasses the stomach and helps in the intestines).
Third-party tested brands (labels like USP, NSF, or Informed Choice).
Standardized extracts when possible, so you know exactly what you’re getting.
This small step dramatically boosts both safety and effectiveness.
4. Watch for Interactions
Even natural remedies can interact with medications. A few examples:
Turmeric/curcumin may thin the blood, so check with your doctor if you take anticoagulants like warfarin.
Licorice root (non-DGL) can raise blood pressure and lower potassium, which is risky if you already have heart or kidney issues. Stick with DGL licorice for digestion instead.
Peppermint oil can worsen reflux for some people if not enteric-coated.
Think of these not as deal-breakers, but as reminders to check in with your clinician before making changes.
5. Pair Herbs with the Basics
Herbs work best when paired with lifestyle foundations that also support gut health:
Eat consistent meals.
Include fiber you tolerate well.
Stay hydrated.
Move your body daily (a short walk counts!).
Practice stress-regulating habits like deep breathing, yoga, or gentle stretching.
These habits make the “gut–brain axis” more resilient — and the herbs can give that extra nudge you need.
A Simple Two-Week “Try-It” Plan
Trying herbs for digestion doesn’t have to be complicated. Think of it as a short experiment — a way to gently test what actually helps your body without changing everything at once. Here’s a simple two-week plan you can follow:
🌿 Week 1: Start with the Basics
Peppermint oil for IBS-type pain or bloating
If cramping or bloating is your main struggle, start with an enteric-coated peppermint oil capsule. These are designed to release in your intestines (not your stomach), where peppermint can calm spasms and ease discomfort.Artichoke leaf or peppermint + caraway for fullness and pressure
If your problem feels more like heaviness or pressure in the upper stomach after meals, try artichoke leaf extract or the peppermint + caraway combo (sold as Menthacarin). Studies show these can lighten that “too full” feeling and improve meal tolerance.Chamomile or lemon balm in the evening
If stress plays into your digestion (and for many people it does), add a calming cup of chamomile or lemon balm tea before bed. Both herbs are gentle, help settle the nervous system, and may ease stress-related stomach tightness.
🍵 Week 2: Layer in Extra Support
Ginger for nausea or queasiness
If nausea still lingers, bring in ginger tea or capsules. Ginger is well-studied for calming queasy stomachs, whether from meals, travel, or other triggers.Fennel + curcumin for stubborn bloating
If bloating remains your main complaint, consider trying a blend of fennel and curcumin (the active part of turmeric). Early research suggests this combo can ease gas and improve gut comfort.
Keep Track as You Go
📝
Every day, jot down a few notes:
How bloated or crampy you feel
How your bowels are behaving
Your stress level
Any side effects
This isn’t about perfection — even a 30% improvement is a win and may show you which herbs are worth keeping in your routine.
FAQs on Digestive Herbs
❓ Can herbs replace my medications?
No. Herbs can support digestion and ease symptoms, but they don’t replace prescription medications. For example, turmeric (curcumin) may help people with ulcerative colitis, but it works best with standard medical care — not as a substitute. Always check with your healthcare provider before making changes to your treatment plan.
❓ What are the best herbs for bloating?
Some of the most studied herbs for bloating include peppermint oil, fennel, ginger, and artichoke leaf extract. Peppermint oil capsules are often recommended for IBS-related bloating and cramps, while fennel and curcumin blends may help with gas and fullness.
❓ Are herbal teas effective for digestion?
Yes, herbal teas can support digestion, especially gentler options like chamomile, lemon balm, and ginger. Teas may not be as strong as standardized extracts used in clinical trials, but they’re safe for everyday use and can still calm stress, ease cramping, and reduce mild nausea.
❓ Is peppermint oil safe for acid reflux?
It depends. Peppermint oil can relax the valve at the top of the stomach, which may worsen acid reflux in some people. That’s why most studies recommend enteric-coated peppermint oil capsules — they release the oil in the intestines, not the stomach, making them safer for people prone to reflux.
